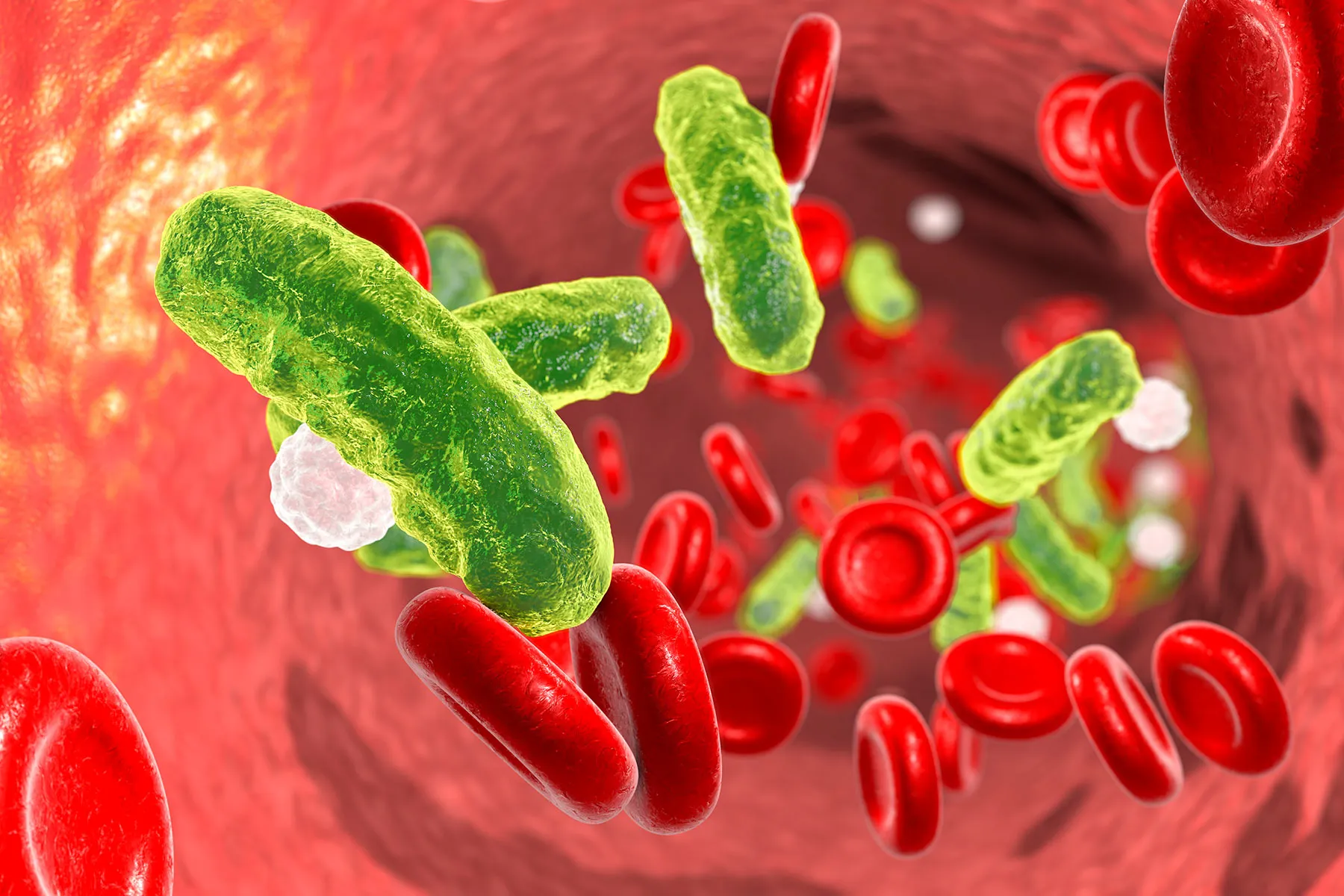
Bloodstream infections (BSIs), also referred to as bacteremia or septicemia depending on severity and clinical context, are serious medical conditions that occur when pathogenic microorganisms enter and circulate within the blood. Because the bloodstream connects all organs and tissues, infections in this system can rapidly progress and become life-threatening if not identified and treated promptly. Understanding the symptoms of bloodstream infections is essential for early detection, timely medical intervention, and improved patient outcomes.
Understanding Bloodstream Infections
A bloodstream infection develops when bacteria, fungi, or, less commonly, viruses gain access to the blood. This can occur through various routes, including infected wounds, urinary tract infections, pneumonia, surgical sites, intravenous catheters, or medical devices. In healthcare settings, BSIs are often associated with invasive procedures or prolonged hospitalization, particularly in immunocompromised patients.
Once pathogens enter the bloodstream, the body mounts a systemic immune response. This response is responsible for many of the characteristic symptoms seen in bloodstream infections.
Early and General Symptoms
The early symptoms of a bloodstream infection are often nonspecific, which can make early diagnosis challenging. These initial signs may resemble common viral illnesses but tend to worsen or persist over time.
Common early symptoms include:
-
Fever or hypothermia: A high fever is a frequent early sign, although some patients particularly older adults or those with weakened immune systems may experience an abnormally low body temperature.
-
Chills and shivering: Often described as rigors, these can be intense and recurrent.
-
Fatigue and weakness: Patients may feel unusually tired, lethargic, or physically weak.
-
General malaise: A broad feeling of discomfort or illness without a clearly localized cause.
These early manifestations indicate that the immune system is responding to a systemic threat rather than a localized infection.
Progressive and Systemic Symptoms
As the infection progresses, symptoms typically become more pronounced and severe. This stage reflects a more widespread inflammatory response and may signal the onset of sepsis, a critical complication of bloodstream infections.
Progressive symptoms may include:
-
Rapid heart rate (tachycardia): The heart beats faster to maintain adequate blood flow and oxygen delivery.
-
Rapid breathing (tachypnea): Increased respiratory rate may occur as the body attempts to correct metabolic imbalances.
-
Low blood pressure (hypotension): A dangerous sign indicating compromised circulation.
-
Confusion or altered mental status: Reduced blood flow to the brain can result in disorientation, confusion, or difficulty concentrating.
-
Decreased urine output: This may suggest impaired kidney function due to reduced blood perfusion.
These symptoms warrant immediate medical evaluation, as delayed treatment significantly increases the risk of organ failure and mortality.
Organ-Specific Manifestations
Because the bloodstream supplies all organs, infections can affect multiple systems simultaneously. In some cases, symptoms related to specific organs may dominate the clinical picture.
Examples include:
-
Respiratory system: Shortness of breath, low oxygen levels, or respiratory distress.
-
Cardiovascular system: Chest discomfort, weak pulse, or signs of circulatory collapse.
-
Renal system: Swelling, electrolyte imbalances, and reduced urine production.
-
Gastrointestinal system: Nausea, vomiting, abdominal pain, or diarrhea.
-
Skin and extremities: Cold, clammy skin, mottling, or bluish discoloration of fingers and toes.
The presence of multi-organ involvement strongly suggests a severe bloodstream infection requiring intensive care.
Symptoms in High-Risk Populations
Certain populations are more vulnerable to bloodstream infections and may present with atypical or subtle symptoms.
-
Older adults: Fever may be absent. Instead, confusion, dizziness, or sudden functional decline may be the primary indicators.
-
Infants and young children: Poor feeding, irritability, weak crying, or temperature instability may be observed.
-
Immunocompromised individuals: Patients undergoing chemotherapy, transplant recipients, or those with chronic illnesses may show muted inflammatory responses, delaying recognition.
In these groups, a high index of clinical suspicion is essential.
Diagnosis and Clinical Evaluation
While symptoms provide important clues, definitive diagnosis of a bloodstream infection requires laboratory testing. Blood cultures are the cornerstone of diagnosis, allowing clinicians to identify the causative organism and guide targeted therapy. Additional tests may include complete blood counts, inflammatory markers, imaging studies, and organ function assessments.
In clinical and hospital supply contexts, antimicrobial agents such as ceftriaxone are commonly discussed due to their broad-spectrum activity. From a pharmaceutical distribution perspective, terms like ceftriaxone injection wholesale are relevant in procurement and supply chain discussions, particularly for hospitals managing high patient volumes. However, clinical use and administration decisions must always be made by qualified healthcare professionals based on individual patient factors and diagnostic findings.
Importance of Early Recognition
Early recognition of bloodstream infection symptoms is critical. Prompt medical intervention significantly improves outcomes by preventing progression to severe sepsis or septic shock. Delays in treatment are associated with increased hospital stays, higher healthcare costs, and elevated mortality rates.
Healthcare providers emphasize patient education, especially for individuals with chronic illnesses or indwelling medical devices, so that early warning signs are not overlooked.
When to Seek Immediate Medical Care
Medical attention should be sought immediately if any of the following occur:
-
Persistent high fever with chills
-
Sudden confusion or difficulty staying alert
-
Rapid breathing or heart rate
-
Very low blood pressure or fainting
-
Signs of organ dysfunction, such as reduced urine output or severe shortness of breath
These symptoms represent a medical emergency.
Conclusion
Bloodstream infections are complex and potentially life-threatening conditions that require rapid identification and management. Symptoms often begin subtly but can escalate quickly, affecting multiple organ systems. Recognizing early warning signs such as fever, chills, fatigue, and confusion can be lifesaving.
From both clinical and healthcare operations perspectives, understanding bloodstream infections is essential. While discussions around antimicrobial availability, including considerations such as ceftriaxone injection wholesale supply, are important for healthcare infrastructure, patient safety ultimately depends on timely diagnosis, appropriate medical care, and professional oversight.
Awareness, vigilance, and early intervention remain the most effective tools in reducing the serious consequences associated with bloodstream infections.